Renal Disease in General Practice
How is renal disease is tested in GP training?
Renal disease is one of the most consistent sources of lost marks in both the AKT and the SCA — not because it’s rare or complex, but because it’s easy to approach in the wrong way.
Trainees often focus on CKD stages, numbers, or new drugs, when exams are really testing something else:
your ability to interpret trends, recognise risk, prioritise management, and explain decisions clearly and proportionately in a GP context.
This resource is designed to help you think about renal disease the way exams expect you to, and the way it presents in real UK general practice — without role-play cases or unnecessary complexity. It is aligned with RCGP renal & urology learning outcomes — including CKD, AKI recognition, cardiovascular risk, and medication safety.
It is relevant for ST1–ST3, and particularly useful if renal questions or consultations consistently feel uncomfortable rather than unfamiliar.
How to use this resource
This pack is structured around five focused learning pillars.
They are designed to work together, but you do not need to complete them in order.
If you already know where your gaps are, you can go straight to the section you need.
You can:
work through everything sequentially, or
dip into a single pillar for targeted revision.
Five Renal Learning Pillars
1. How renal disease is actually tested (AKT & SCA)
Why trainees lose marks — and what examiners are really looking for.
2. CKD thinking (not stage memorisation)
How to interpret eGFR, trends, and ACR in a GP-relevant way.
3. Medications and renal disease
ACE inhibitors, statins, sick-day rules — and common exam pitfalls.
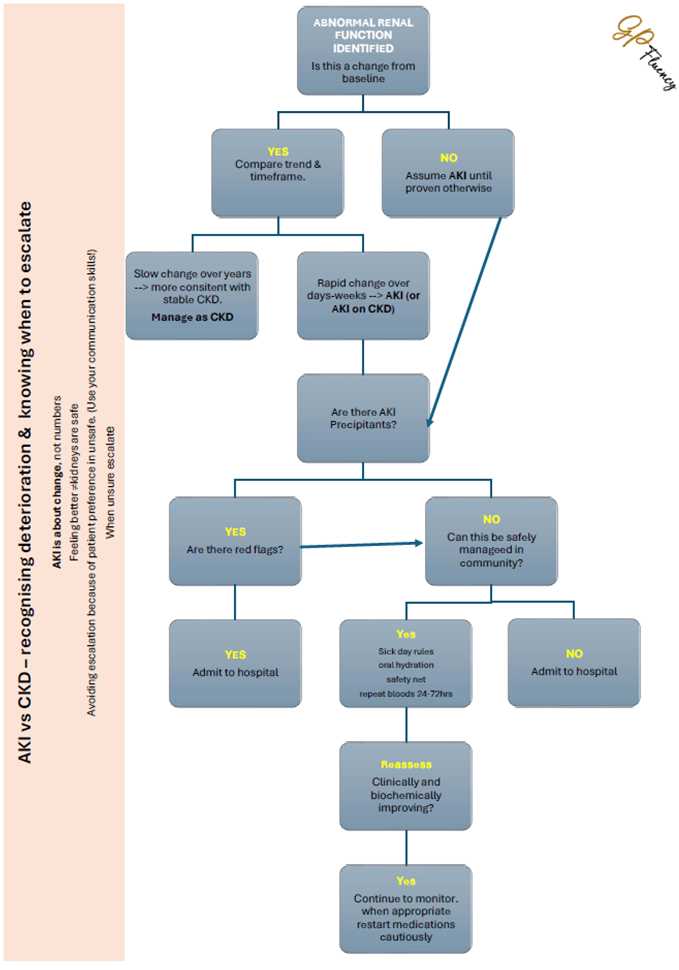
4. AKI vs CKD and escalation decisions
Recognising deterioration and knowing when community management is unsafe.
5. Exam pitfalls and renal reasoning with vignettes
Short, written scenarios and AKT-style questions to practise judgement (not role-play).
Pillar 1: Renal disease in exams:
Start here.
This short PowerPoint sets the scene for the rest of the renal resource. It explains how renal disease is tested in the AKT and SCA, why it often catches trainees out, and what examiners are really looking for.
It’s designed as a quick mindset reset — you can work through it in a few minutes, then dip into the other pillars depending on where your learning needs are.
Pillar 2: CKD thinking - stop memorising stages
CKD in GP is not about the stage label
In GP exams — and in real practice — chronic kidney disease is rarely assessed by asking what stage it is.
What matters is what that kidney function means for this patient, over time, and what you do about it.
A single eGFR value rarely tells you enough.
-
Why does a raised ACR change management?
A raised urine ACR indicates protein leakage from the kidneys, which is a marker of ongoing kidney damage and increased cardiovascular risk.
Because of this, NICE guidance expects earlier and more active intervention when ACR is raised.
How ACR changes blood pressure management
When urine ACR is raised:
Blood pressure becomes a key driver of kidney and heart outcomes
Tighter BP control is recommended
Even mildly elevated blood pressure may warrant treatment
Without proteinuria, stable CKD can often be monitored conservatively.
With proteinuria, the kidneys are at higher risk of progression, and blood pressure management becomes more urgent.How ACR changes ACE inhibitor / ARB use
A raised ACR:
strengthens the indication for ACE inhibitors or ARBs
even when blood pressure is only mildly raised
In this context, ACEI/ARBs are used for:
renal protection, not just BP control
reducing proteinuria
slowing CKD progression
lowering cardiovascular risk
How this is tested in exams
AKT
Raised ACR often shifts the best answer towards:
starting or optimising ACEI/ARB
tighter BP control
SCA
You may need to explain why treatment is recommended despite only mild BP elevation:
“The protein in the urine tells us the kidneys are under strain, so controlling blood pressure becomes more important.”
Key takeaway
Raised ACR lowers the threshold for action.
It turns CKD from something that can often be monitored into a condition where active risk reduction is needed.
-
Renal disease is one of the areas where trainees are most likely to make unsafe assumptions about medication — either stopping drugs unnecessarily or missing high-value preventative treatment.
Exams are not testing drug recall.
They are assessing whether you understand risk, benefit, and prioritisation in the context of kidney function.Start with this principle
In CKD, the most important medications are often protective — not harmful.
Many renal-related exam errors come from over-caution, not recklessness.
-
What examiners expect you to know
A small rise in creatinine after starting is expected
ACEI/ARBs are renal-protective, particularly in:
hypertension
raised urine ACR
They reduce:
progression of CKD
cardiovascular risk
When to be cautious or stop
Significant AKI
Severe hyperkalaemia
During acute dehydration (sick-day rules)
Common exam pitfalls
❌ Stopping ACEI because creatinine has risen slightly
❌ Saying “it can damage the kidneys” without explaining benefit
AKT tip:
A mild creatinine rise is rarely the best reason to stop an ACEI.SCA tip:
You should be able to explain why this drug protects the kidneys in plain language. text goes here -
What matters
Increase risk of:
dehydration
AKI during intercurrent illness
Common contributor to AKI on CKD
Exam expectations
Recognise when diuretics worsen renal function
Apply sick-day rules appropriately
Balance volume status, not reflex stopping
Exam pitfall:
❌ Ignoring diuretics when AKI is present
-
Key knowledge
Generally safe in stable CKD
Must be stopped temporarily during:
acute illness
dehydration
AKI
Why this matters in exams
Lactic acidosis is rare but exam-relevant
Metformin often appears as a safety discriminator
Exam pitfalls:
Forgetting metformin when discussing sick-day rules. -
This should be automatic
Avoid in CKD
Avoid during dehydration
Particularly risky with:
ACEI/ARB
diuretics
(“triple whammy”)
Exam pitfall
❌ Recommending NSAIDs for pain in CKD without comment
-
Core expectation
CKD significantly increases cardiovascular risk
Many CKD patients will have:
QRISK3 ≥10%
Statins are preventative, not symptom-based
What good answers do
Link CKD to heart risk
Justify statins even when the patient “feels fine”
Exam pitfalls
❌ Avoiding statins because of CKD
❌ Failing to calculate or acknowledge QRISK3
Key point:
CKD is often a reason to start a statin, not stop one. -
Sick-day rules: medications to temporarily stop during acute illness
Sick-day rules apply when a patient is acutely unwell, particularly with:
vomiting or diarrhoea
fever
poor oral intake
dehydration
suspected AKI
The aim is to reduce the risk of acute kidney injury and electrolyte disturbance.
ACE inhibitors / ARBs
(e.g. ramipril, lisinopril, losartan)
Why stop temporarily
Reduce renal perfusion during dehydration
Can worsen AKI
Risk of hyperkalaemia
When to stop
Acute illness with dehydration
Vomiting/diarrhoea
Poor fluid intake
When to restart
Once eating and drinking normally
Usually 24–48 hours after recovery
Consider checking renal function if illness was severe or prolonged
Diuretics
(e.g. furosemide, bendroflumethiazide)
Why stop temporarily
Increase fluid loss
Worsen dehydration
Increase risk of AKI and hypotension
When to stop
Acute illness with:
vomiting or diarrhoea
reduced intake
signs of dehydration
When to restart
When hydration is restored and symptoms resolve
Restart cautiously if elderly or frail
Metformin
Why stop temporarily
Increased risk of lactic acidosis in:
dehydration
AKI
hypoxia
When to stop
Any acute illness causing:
dehydration
reduced intake
AKI risk
When to restart
Once eating and drinking normally
Renal function recovered to baseline
Exam expectation:
Trainees should remember to include metformin when discussing sick-day rules.NSAIDs
(e.g. ibuprofen, naproxen)
Why stop / avoid
Reduce renal blood flow
Increase AKI risk
Particularly dangerous with:
ACEi/ARB
diuretics
(“triple whammy”)
When to stop
Any acute illness with dehydration
Ideally avoided altogether in CKD
When to restart
Generally avoid restarting in patients with CKD
Use alternative analgesia where possible
How this is tested in exams
AKT
Knowledge of which drugs to stop
Understanding why, not just memorisation
SCA
Clear explanation in plain language
Appropriate safety-netting:
“Once you’re eating and drinking normally again, you can restart these — if you’re unsure, check with us.”
-
These are not first-line CKD treatments
What examiners expect:
Awareness that they exist
Understanding they are add-on therapies for use after the patient is already on optimised standard therapy (Good BP control, ACEI/ARB) – it is not a substitute
Recognition they are used in selected patients (CKD 2-4 with increased renal or cardiovascular risk with raised urinary ACR and diabetic or nondiabetic CKD with proteinuria)
What examiners do not expect:
Early or enthusiastic suggestion (An SCA temptation for some)
Replacement of ACEI/ARB
Use without clear indication
Exam warning:
Over-emphasising SGLT2 inhibitors is a common trainee error.It is possible to think you’d be expected to discuss dapagliflozin in the SCA, but it is unlikely and it is strongly recommended trainees ensure it is indicated and all other management has been optimised first (and in day-to-day general practice this applies too)
-
Before answering any renal medication question, ask:
Is this drug protective or harmful in this context?
Is the kidney problem stable or acute?
Does this patient have raised cardiovascular risk?
Am I stopping something because it’s unsafe — or because I’m uncertain?
Strong answers show intentional prescribing, not blanket caution.
Pillar 3: Medication & Renal Disease
Click on the plus signs to learn more about each heading.
Prefer everything in one place - click here to download the Medication & Renal Disease pdf.
Pillar 4:AKI vs CKD – recognising deterioration & knowing when to escalate
AKI is about change, not numbers
Feeling better doesn’t mean kidneys are safe
Avoiding escalation because of patient preference is unsafe. (Use your communication skills!)
When unsure - escalate
Click here for a downloadable flow chart to put in your doctors office/bag
Pillar 5: Exam pitfalls and renal reasoning
This section brings together the key learning from the renal resources and pillars 1-4. It focuses on how to demonstrate your knowledge and skills of renal disease and it’s management when it is assessed, both in practice and in exams.
As you click through the slides here, you’ll work through a small number of short reasoning vignettes and AKT-style questions, designed to help you practise clinical prioritisation and judgement rather than recall or role-play.
Each explanation highlights common exam pitfalls and signposts you back to the relevant pillar if you want to revisit the underlying thinking. The emphasis throughout is on recognising risk, choosing proportionate management, and explaining decisions clearly — the skills expected of a safe, independent GP.